Until the racism is over, a framework for empathy
This post was originally published by my colleagues at PK on June 15, 2020

Nobody knew that 2020 would be the year the word “unprecedented” would become exhausted from overuse. But as I write this, sixty million Americans are living under curfew due to civil unrest, the most since Dr. King’s assassination. My neighbor’s three-year-old daughter, who barely understands the social distancing of the pandemic, says she now wants to stay inside until racism is over too. That’s the year we’re having together.
We are entering a world of trauma-informed marketing and design
These months have exacerbated the effects of institutional racism and inequality, bringing millions to the point of desperation. Experts say that the psychological and societal injuries of this time may themselves become shadow pandemics lasting beyond the arrival of a COVID-19 vaccine.
Fortunately, forward-looking hospitals have dramatically expanded their mental health services; they’ve also been working to lower the stigma of mental healthcare. Those of us who engineer the mechanics of healthcare experiences will need to be far more attuned to the stressors which define huge parts of consumers’ lives.
In my teaching and work, I’ve started to use the abbreviation SIMI: stress, illiteracy, mistrust and inequality as a way to keep the obstacles to engagement which people must struggle against in mind. It’s one way to help teams to focus on human empathy before engineering solutions.
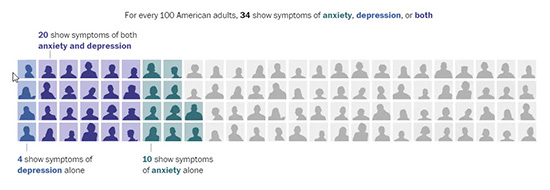
Stress
Almost every day the news brings fresh studies indicating the high baseline of stress that American consumers currently face. This week, the US Census reported that one-third of Americans now show signs of clinical anxiety or depression.
The effect of civil protests and social isolation on children’s mental health is impossible to know. However, researchers from the University of Bath conducted a meta-study concluding young people are as much as 3 times more likely to develop depression in the future due to social isolation, with an impact on mental health lasting up to 9 years.
Illiteracy
Along with the devastating influence of stress, we must recognize the growing barrier of literacy. Half of Americans read at or below a seventh-grade level, according to a report by The Program for the International Assessment of Adult Competencies (PIAAC), while only two percent read above an 11th-grade level. This is a big problem because so much healthcare content is written at a level that would frustrate the average reader.
This same report shows that reading ability in the US has experienced a gradual, thirty-year-long decline. Understanding insurance claims and processes, medication doses and diagnoses can be challenging regardless of reading level, but the challenges are exacerbated by limited literacy. Healthcare communicators may develop more video and voice over resources to reduce reading and continue to translate materials for non-native readers.
Mistrust
The healing alliance of healthcare is rooted in trust. After all, many healthcare services are what we’d call credence goods. This means that one may not know if they needed or benefited from a service, even after receiving it. Add to this, a financial opacity amplified by secret rate agreements between payers and drug companies—and there’s an experience gap that that drives mistrust. Consumers are losing trust in the healthcare industry.
In 1975, 80% of the public had confidence in the healthcare industry. In 2018 only 34% of the general public told Gallup that they had a positive view of the industry. There’s been an erosion of authority which perhaps goes with media changes and the digital world. While there’s a natural denial from fear of treatment, it’s exacerbated by the idea that any of us could end up soliciting donations online when the cost of care outstrips our resources. Healthcare faces a toxic cocktail of mistrust, and that’s a constraint we must work against.
Inequity
Finally, as we conduct primary research with patients, they are profoundly concerned about inequality and fairness in healthcare access. Just this week, an NPR investigation found that in four out of six of the largest cities in Texas testing sites were disproportionately located in whiter neighborhoods. This is just one of the structural inequities making COVID-19 more deadly among racial minorities. Healthcare brands can’t remain silent about improving equality of access – this is becoming a politically and culturally charged topic.
Stress, illiteracy, mistrust and inequality are powerful forces — but they are mostly outcomes of cultural systems that we can improve. In fact, three hospitals we admire are marshaling their creativity and resources to lower stigma and expand their mental healthcare services.
Nationwide Children’s, Colorado Children’s and McLean Hospital are working to end stigma and expand mental health resiliency
Nationwide Children’s has launched a major behavioral health facility, leading them to recruit mental health staff in a home page call out, and they continue their compelling On Our Sleeves content hub to fight mental health stigma.
Nationwide has also developed a community resource finder, which mirrors their doctor finder, but instead is full of mental health resources available across the communities they serve. And they are staffing up to provide increased resources, which the COVID lockdown and economic disruption will predictably bring.
Children’s Hospital Colorado is building facilities, fighting stigma and advancing research
An estimated 226,000 kids and teens in Colorado have diagnosable mental health conditions, yet only 21 percent receive professional care. And tragically, suicide is the leading cause of death for young people age 10-24 in that state.
As a Denver native, I’m proud that Colorado Children’s is campaigning to get every child in their state the mental health support they need.
McLean Hospital is deconstructing stigma
Despite the concerns of being labeled and risking stigma, 75 volunteers have shared their stories of hope and resilience in public installations around Boston, and on a website that’s reminiscent of Nationwide Children’s On Our Sleeves project.

Several of the volunteers are famous, but all of them feel familiar. It’s a chance to “walk in their shoes” and appreciate the growth and healing possible with care.
Stress, illiteracy, mistrust and inequity are barriers patients must overcome in their journey to care. Strategies to engage health consumers must recognize the context these create, and advocate to address the social deficits which are their cause.
We have closed the US economy to compensate for a health system unprepared for a pandemic. Now it’s time to address the inequities that have made the burden of COVID-19 fall disproportionately on minority and lower-income communities.
As we make sense of the global trauma of 2020, making mental health a primary measure of national well-being could be a smart change. One lesson of this time may be that humanity needs much more than GDP alone. That might be enough to take care of business, but we need new top-level goals to care for each other as well.
 The future of digital experiences will be built by strategists who grasp the full array of emerging business, social, and technical models. Specialties in user experience, branding, application design, and data science are laying the foundation for richer user experiences and business models breakthrough products and revenue based marketing.
The future of digital experiences will be built by strategists who grasp the full array of emerging business, social, and technical models. Specialties in user experience, branding, application design, and data science are laying the foundation for richer user experiences and business models breakthrough products and revenue based marketing.
33 Responses to "Until the racism is over, a framework for empathy"
July 14, 2020
Nice write-ups thanks for sharing! |
July 14, 2020
Great article! Thanks
July 14, 2020
I love the information. Thanks for sharing!
July 14, 2020
You have a great article. Thanks!
July 20, 2020
Worth the time and read! Thanks!
August 13, 2020
Indeed, the lack of empathy on the part of white Americans has long impeded the fight for racial equality.
August 24, 2020
Thanks for the share.
August 24, 2020
Glad to see this great content.
September 4, 2020
Worth the time I spent reading your article. You have such a great idea. Thanks a lot!
September 8, 2020
We should cut this stigma off. This should end.
September 8, 2020
This has been on for years now. I wonder why we only take fewer actions.
September 30, 2020
Worth to read. Thanks for sharing!
October 12, 2020
great read. worth reading
October 12, 2020
very cool read
November 14, 2020
Thank you for this!
November 22, 2020
You’ve done a really great job in sharing this!
November 27, 2020
Im happy that they are doing something about this issue.
November 27, 2020
Let’s do our part and put an end to racism.
December 10, 2020
We should all stop racism.
December 31, 2020
This is great content.
May 7, 2021
Thank you for this very informative post!
August 12, 2021
Very interesting post!
August 26, 2021
[…] This week, Healthcare Business Today, previewed a longer guide to Consumer Loyalty in Healthcare I’ve been working on with my PK Global co-worker, Stephanie Cohen. It starts with a case study I’ve taught from at Rutgers the last few years, and cites some provocative polling about erosion of trust in healthcare, which got me thinking about how to a pandemic need for empathy. […]
June 20, 2022
Wow, I love it! Thank you so much for sharing
August 11, 2022
Interesting article thank you for sharing check article here 800 Stock Law
September 9, 2022
Very informative, Congratulations!
Greetings from Tree Removal Near Me
September 9, 2022
Good to hear, many child will be happy with this project Here
September 14, 2022
This sounds promising, great! https://www.grandrapidsgeneratorservices.com/
September 14, 2022
Definitely worth reading, this will take my time while waiting for my friends https://www.iowacityconcretecontractors.com/
November 25, 2022
Thank you for taking the time to share this with us.
March 27, 2023
Those of us who engineer the mechanics of healthcare experiences will need to be far more attuned to the Bollard installation Pasadena and stressors which define huge parts of consumers’ lives.
May 11, 2023
I totally agree with this blog discovergrandmesa.com
November 10, 2023
Great. Thank you for sharing this. ESW0009